Hannah – A Student in CancerLand

I like being a student. Learning is something I never get tired of. The work I did as an undergraduate student in a neuroscience lab, as well as getting my master’s degree in library science set me up to be a lifelong learner, but in a way, I did not expect. About six years after I finished my secondary education, I was hurled into CancerLand as a patient who could not sit idly — I became a student of a different kind.
In the first part of 2016, I was diagnosed with Stage 1 breast cancer (HR+, HER2-). I had two little children, no major risk factors, and a generally healthy lifestyle. Becoming a patient was a new role for me, and boy did I have a lot to learn. After surgery, chemotherapy, and radiation were finished, I thought, “Hurray, I can put this behind me and move on!” But clearly, I hadn’t learned that once a patient is touched with cancer, it’s never too far behind you — whether that be a mental state or physical manifestation of the disease itself. In fact, for many of us, it comes back again (if it ever went away at all) in the form of metastatic breast cancer (MBC).
In 2018 life was just beginning again for me after my early stage treatment was completed. I traveled with my family, celebrated a wedding, had a relatively new job, my kids were entering school, my husband and I were bringing to reality the things we put on hold while dealing with cancer treatments, and we were creating a community of wonderful friends around us. But then I found a lump on my sternum — one thing led to another and I was diagnosed with MBC to my bones and one spot in my lungs. I was sent back to being a student again…I had a lot to learn.
I navigated through something unimaginable at age 33 by spending countless hours reading research papers, learning about my disease, talking to my doctors, etc. In that first year, I started planning for the end of my life as I knew it. Nothing could ever be the same, right? As time passed, and that first hard year slipped behind me, I was accepting my cancer reality and living a full life doing things I loved -knitting, studying genealogy, traveling, making plans with friends, cross-country skiing, paddle boarding, walking in the woods, cooking, etc.
The part of CancerLand I wanted to be a part of the most was research. I said yes to any opportunity I could to participate in research — from drug trials, to side effect management, to blood tests for cellular research. Being involved in and up to date on research was something that kept me learning, evolving, and hoping for better disease management, and maybe someday a cure.
Early last summer, I decided to take part in a study at Brigham and Women’s Hospital that was looking at whether or not adding brain MRIs to standard of care would help in early detection and treatment of brain metastases if they were to occur during MBC disease management. For me, at that point, I had progression to my liver, but no indication of brain metastasis. From my research as well, because of my subtype, I was at very low risk of ever developing brain mets. Spoiler alert…I am writing this blog entry on MBCBrainMets.org for a reason 😉
The screening MRI results came back showing a couple of very small brain mets in the back of my brain. I was shocked and so sad to learn of this progression, but also determined to again be my best advocate and learn all I could so I could get back to living. And after doing a full brain and spine MRI I was told that I didn’t just have those little spots on my brain, but I was also living with leptomeningeal disease (LMD). This, I would come to find out, is cancer that is in the cerebral spinal fluid. I had never heard of this before.
With this news, I was plunged back into student mode. I felt like I was learning about a brand new cancer type for the first time. It felt like I was back in the first year of my MBC diagnosis — just barely being able to come up for air, gathering so much information, and realizing just how rare LMD is and how difficult it is to treat. I was low, but I wasn’t without hope. I felt empowered to figure out how I was going to treat this new uninvited CancerLand resident.
I poured my worries and sleepless nights into researching LMD. I knew I wanted to do radiation, and specifically proton therapy. Proton therapy requires a special proton machine, and there aren’t many facilities around the US, plus I was advised not to fly. But I was also told I needed to start treatment quickly, so I agreed to whole brain radiation (WBR) in Boston, and started working on looking for someone to do proton therapy to my spine. I found a facility in NJ that could and would do it. After five daily WBRs were completed, I made plans to head down to NJ (6 hours away) to complete ten daily proton radiation treatments.
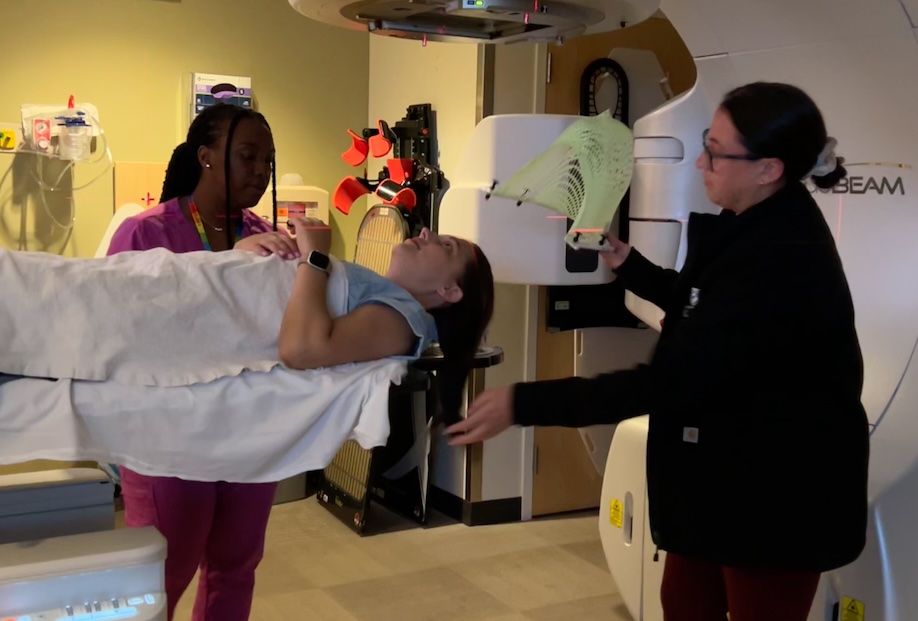
Radiation to my brain and spinal cord was a lot like traditional radiation to the breast, but it also had its own unique features. WBR (which used photons) and proton therapy required a special mask to be made to stabilize my head and neck. The mask is quite cozy and required a lot of deep breathing on my part to get past any inkling of claustrophobia, which I don’t usually have. I also had to get small dot tattoos on my hips and abdomen for the proton therapy so that my spine would be in the exact same location each session.
Once the mask was on, WBR sessions were quick and easy – lasting less than a minute; each session of proton therapy was a bit longer – lasting 5-10 minutes each. The side effects of WBR didn’t hit until about a week or so after my treatment course was complete. I experienced hair loss, fatigue, numbness in my toes, balance issues, unusually slow thinking/processing, forgetfulness, and basically any ability to multitask. Everything I did from thinking to walking required deliberate attention. These side effects lasted most intensely for about 4-6 months. I still have numbness in my toes that I don’t believe will ever go away. Since the proton therapy was focused on my spine and spinal fluid I didn’t notice any changes like I did with WBR, with the exception that I had drier skin along my spine, which darkened over time, but never burned.
While I was doing radiation and after, I couldn’t just sit back and recover. I needed to know what was next for me. LMD as a disease is treated almost as if it’s a separate cancer because it doesn’t often respond well to treatment and it can progress extremely rapidly. So I started to talk to specialists who had experience with LMD and made a plan to even start a treatment that was invasive and intense to treat the LMD if it didn’t respond to radiation.
The good news is that my LMD has responded extremely well so far to the radiation (9 months out). It has shrunk and stabilized while being on systemic chemotherapy. I attribute so much of my success with treatment to educating myself on my disease and my treatment options. My love of learning has served me well.



