Terry Cohen – Living Life with Brain Mets
Yes, it is malignant
Just as with my early-stage cancer diagnosis, my diagnosis of metastatic cancer and then brain Mets took quite a while. In each case, we weren’t quite sure what I had.
I was diagnosed and treated for stage one breast cancer in 2003. All was well until 11 years later when I started having neck pain. MRIs showed something, but they weren’t quite sure what it was. My oncologist did not think that it was metastasis since it doesn’t often present in the cervical spine, but that’s what it turned out to be. So now I was stage 4 with bone metastasis. I learned to live with uncertainty after these diagnoses.
My first brain MRI
A few months into the treatment I decided to attend the Living Beyond Breast Cancer conference for people with metastatic cancer. I didn’t know anyone else with this disease and wanted to meet people and learn as much as I could. It was a fantastic event, and I met a group of women that became friends and great sources for support. Unfortunately, most of these wonderful women are no longer here, and I miss them very much.
Back to the hotel
I woke up in the middle of the night and felt that the back of my head was sticky. I got out of bed and realized I was bleeding. I woke up my boyfriend all panicked. We think I must have hit my head on the nightstand. I freaked out worrying that maybe I hit my head worse than I thought, so we decided to go to the nearby hospital. The doctor at the hospital gave me a simple stitch. I called my doctor the following day, and she set an appointment with a neurologist who ordered an MRI. What I didn’t know was that my doctors were concerned that perhaps I had a seizure. The MRI ended up showing a little spot that would not have caused a seizure. The next MRI was a few months later and showed that it shrunk. They said that means it’s either not a Met or the Xeloda is working, however, it reemerged in the following MRI and was larger. I was advised by my neuro team to get rid of it. They recommended SRS (stereotactic radiosurgery), which enables a high dose of radiation to be pinpointed to a single spot.
SRS treatment
The radiation is composed of hundreds of beams, but they have too small of a dose of radiation to hurt or impact other parts of the brain. What makes this work so brilliantly is the system can be programmed to make sure that the beams only intersect at the location of the tumor, where they now have a dosage high enough to impact the tumor. The former physics major in me was highly intrigued.
For this to work, your head must be perfectly still. This is accomplished in various ways depending on the system used and where you are treated. At my hospital, they use a mask that is customized to your face. The bottom of the mask is screwed into the machine. Once you have a custom mask, you wear it, and it is also screwed into the bottom mask.
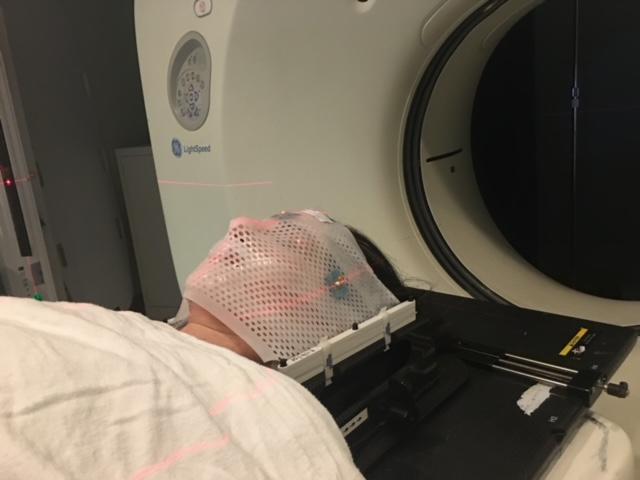 Getting the mask made was no picnic. I felt it hard to breathe and swallow and couldn’t wait to get it off.I got used to it pretty fast, which is lucky for me since I’ve used it multiple times since that first time. This is a picture of me right before my first SRS radiation. I was nervous about the side effects, but otherwise, I was comfortable and okay with the mask. I can imagine that claustrophobic people may have a hard time getting used to this.
Getting the mask made was no picnic. I felt it hard to breathe and swallow and couldn’t wait to get it off.I got used to it pretty fast, which is lucky for me since I’ve used it multiple times since that first time. This is a picture of me right before my first SRS radiation. I was nervous about the side effects, but otherwise, I was comfortable and okay with the mask. I can imagine that claustrophobic people may have a hard time getting used to this.
Here I am after it was over, sending a pic to family and friends.

Ongoing treatment
My main side effect was fatigue. It’s now been over seven years since then, and I’ve had multiple SRS sessions. They typically would break the SRS session into three sessions. In general, it seems to work well for me in that the targeted mets will either shrink, disappear or stabilize. My biggest concern now is wondering how long can I continue to zap away the new mets as they arrive? How can we prevent them from arriving in the first place? I’m looking at new medications that may help make a difference for brain mets.
I recently participated in a clinical trial with Immunotherapy (Pembrolizumab) and SRS. The theory is that the immunotherapy if taken right before the SRS could enable an immune response against the nontargeted mets. So, for the trial, the radiation targets some mets and we look to see if other mets nearby are stabilizing or reducing, etc. I had some success with it, but I am no longer on the trial since I had a progression with one of the nearby mets.
My recommendation to everyone is to keep yourself knowledgeable. Keep learning about possible treatments. It does help to learn how to live with ambiguity because there are not always clear answers.
I wish everyone much success with their treatments. Here’s to living life with brain mets!




