Understanding leptomeningeal disease
Breast cancer can spread not only to the brain, but to the inner layers of tissue that line the brain and spinal cord, known as the leptomeninges. Also known simply as “lepto.”
Breast cancer can spread not only to the brain, but to the inner layers of tissue that line the brain and spinal cord, known as the leptomeninges. Also known simply as “lepto.”
Breast and lung cancer are among the most common cancers which may lead to LMD. This type of cancer is also called leptomeningeal carcinomatosis, carcinomatous meningitis, LMD, and/or lepto. The leptomeninges protect the brain and spinal cord, and they are bathed in cerebrospinal fluid (CSF) which serves as an extra cushion of protection. Leptomeningeal disease is different from other metastasis from breast cancer because it does not form a solid mass. Rather, the cancer floats and/or thickens in the fluid around the brain and spinal cord.
It is important to distinguish metastasis involving the leptomeninges from metastasis involving an outer layer of the meninges, called the dura mater or pachymeninges. Pachymeningeal involvement has a different prognosis than leptomeningeal involvement and the treatment options are also very different.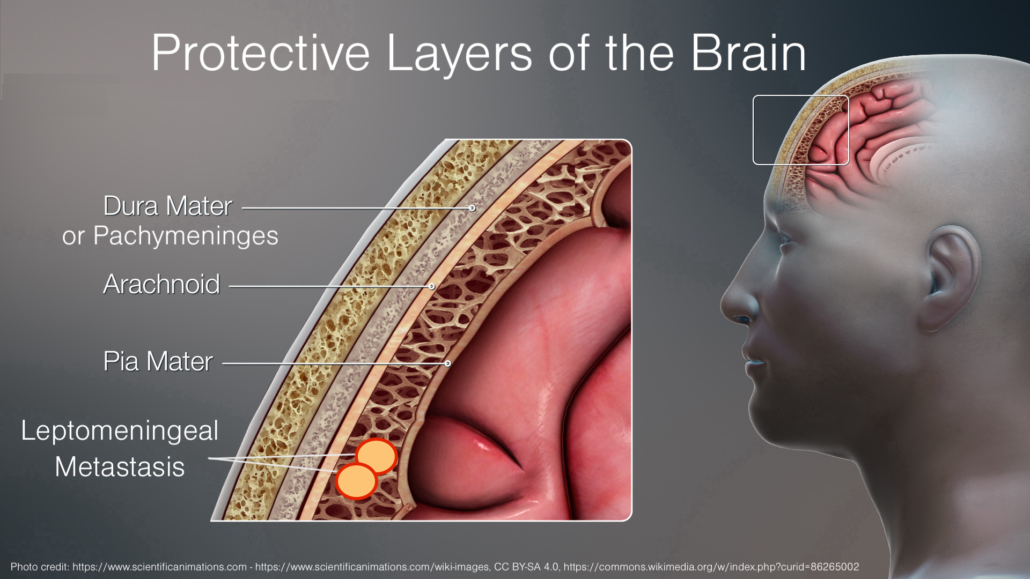
Recognizing Symptoms
The symptoms of leptomeningeal disease (LMD) can be similar to those of brain metastasis but will largely depend on where the leptomeningeal metastasis is located. Symptoms that suggest cancer has spread to the leptomeninges include:
While leptomeningeal metastases do not form solid masses, cancer cells can cluster and lodge into the areas around the brain and/or spinal cord.
When leptomeningeal metastasis is present in the fluid that surrounds the brain, patients will experience symptoms that can affect the function of the cranial nerves. These nerves allow a person to 1) see, smell, and hear; and to 2) move the muscles in the face, head, and neck. Therefore, LMD can also cause facial numbness or weakness, difficulty with speech, difficulty chewing or swallowing, double vision, hearing changes, dizziness, and/or seizures.
When leptomeningeal metastasis is present in the fluid that surrounds the spinal cord, patients may experience symptoms that affect the nerves that run the length of the spinal cord from the neck, to the thoracic/chest area, to the lower back, and to the tailbone. These spinal nerves control muscle movement, sensation, and functions of internal organs like the bladder and intestines.
Therefore, symptoms of LMD around the spinal cord may include a lack of coordination in the arms and legs, difficulty walking, weakness, numbness, or tingling in the limbs, and/or loss of bladder or bowel control.
Because the cerebrospinal fluid (CSF) is constantly circulating, leptomeningeal metastasis can be present around both the brain and spinal cord which can result in fluid build-up that increases the pressure in these areas and can cause headaches, nausea, or vomiting.
Diagnosing Leptomeningeal Disease
There are two methods by which a clinician can diagnose leptomeningeal disease (LMD) including 1) testing of the cerebrospinal fluid or CSF and 2) magnetic resonance imaging (MRI). The gold standard for diagnosing LMD is to test the CSF around the spine for the presence of cancer cells. The CSF can be accessed by a lumbar puncture, also known as a spinal tap which involves the insertion of a hollow needle into the space that surrounds the spine in the lower back. The fluid withdrawn from the lumbar puncture will be tested to determine if any cancer cells are present.
Before the lumbar puncture, the patient receives a local injection (shot) of an anesthetic to numb the site where the needle will be inserted, which makes the procedure very tolerable for most patients. More than one lumbar puncture may be required to accurately diagnose LMD, because the CSF is constantly circulating and cancer cells can be difficult to find.
The other method used to diagnose LMD is based on imaging, typically magnetic resonance imaging (MRI) of the brain and/or spine. The EANO-ESMO clinical practice guidelines define four different types of LMD based on MRI patterns that are classified as 1) type A (linear), 2) type B (nodular), 3) type C (both linear and nodular) and 4) type D (neither linear nor nodular). If the imaging is conclusive in the opinion of the treating team, a lumbar puncture may not be totally necessary. Sometimes, even if the imaging is conclusive, a lumbar puncture may be considered so that your clinicians can note the pressure of the CSF, particularly if symptoms such as blurred vision, cognitive changes, urinary leakage, trouble walking, or severe headaches are present. If the CSF pressure is elevated, your clinicians may recommended treatment to lower or relieve the elevated pressure.
An assessment of clinical symptoms can also be used together with CSF cytology and imaging to help guide the diagnosis of LMD.
Any type of breast cancer can spread to the leptomeninges, but patients with HER2+ breast cancer and TNBC have a higher risk of developing LMD. Patients with lobular breast cancer, which forms in the milk-producing lobules instead of the milk ducts, are also at higher risk of LMD.
How long can I live with leptomeningeal disease?
Survival for patients with leptomeningeal disease remains poor and averaging 3-6 months from time of diagnosis. However, there are patients who survive longer, so it is important to remember that each patient is unique and these statistics do not capture all the variations for each individual patient. Breast cancer patients with leptomeningeal disease have lived beyond what the statistics show.
Studies have also shown that specialized care known as palliative or supportive care, which help address the symptoms and stress of an advanced disease, can help manage symptoms and improve quality of life. In some cases, the involvement of palliative care can even extend survival. For patients with leptomeningeal disease, palliative radiation therapy is often prescribed to relieve symptoms of pain or difficulty walking.
Learn more about radiation therapy
Palliative care is provided by a special team of doctors, nurses, social workers, and other specialists who work together to provide an extra layer of support beyond simply keeping the patient alive. Palliative care specialists can help patients get relief from symptoms that include:
Specialists can also assist with psychosocial support by recommending a licensed therapist or offering resources for relaxation techniques including yoga, meditation, music therapy, art therapy, and others. Spiritual support may also be offered to patients who are seeking to be connected with hospital chaplains or local religious and spiritual leaders to help with loss of faith or hope. Lastly, palliative care specialists can assist with explaining complicated medical information, which can reduce confusion or concern around making important treatment decisions.
If you are not already connected with a palliative care provider, ask your treating physician about being connected to a palliative care team
Treatment Options
Treatment options for breast cancer patients with leptomeningeal disease often include oral or IV chemotherapy, radiation therapy, or some combination of these interventions.
Learn more about treatment options for leptomeningeal disease
Explore brain metastasis and treatments
Explore our frequently asked questions
The information on this website is intended for general knowledge only and is not a substitute for medical advice or treatment. The content for this website has been reviewed by our medical advisory board who are experts in the field.